Wirelessly-powered ‘smart bandage’ could provide drug-free wound care
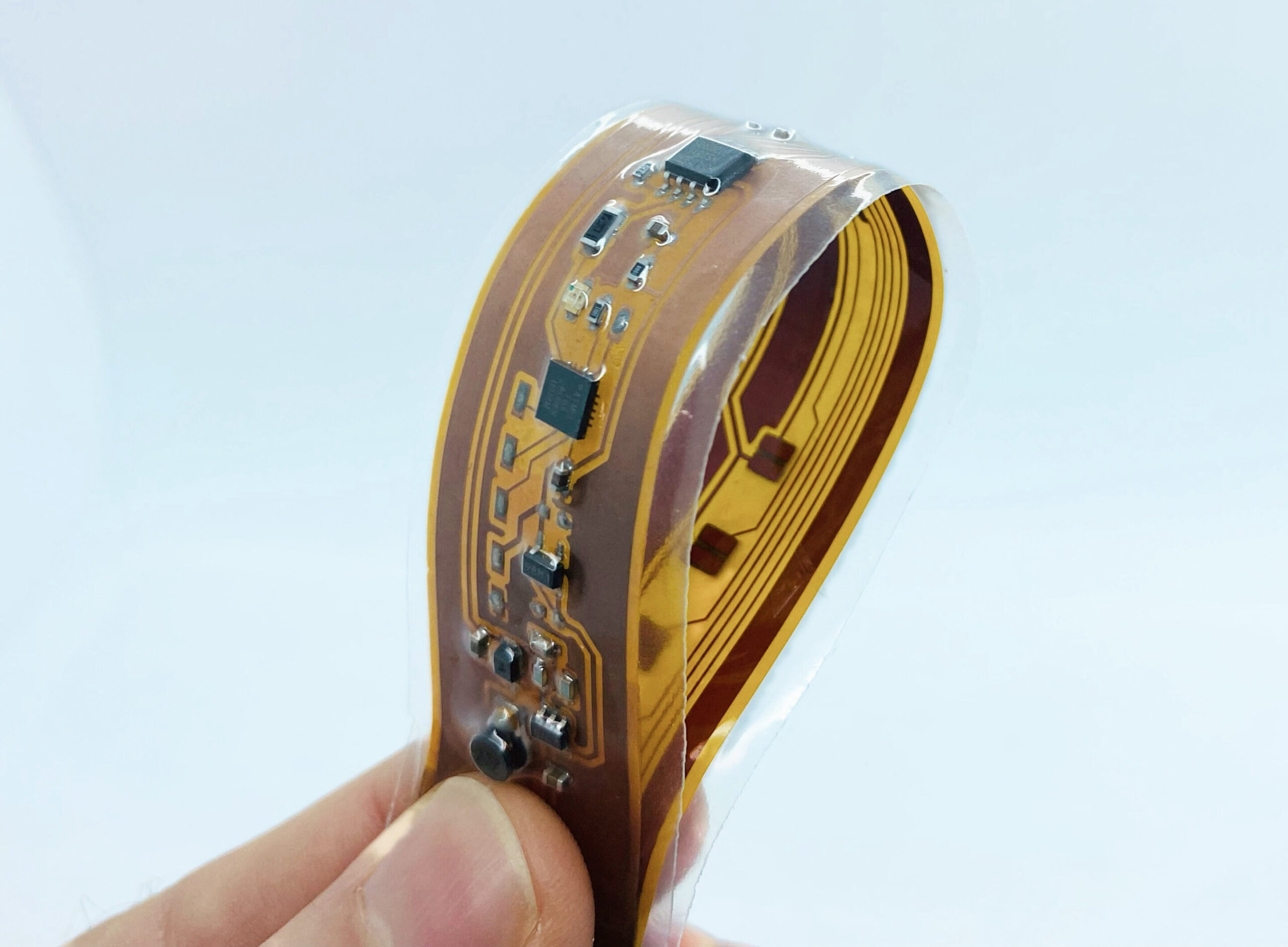
In a path breaking development, a team of scientists at Glasgow University and other universities in Europe have developed a unique bandage that uses the sterilising effect of ultraviolet rays to heal wounds.
According to a press statement, a team of researchers from the UK and France have developed the first-of-its-kind bandage, which is embedded with light-emitting diodes (LEDs) to bathe wounds in sterilising ultraviolet light, preventing the growth of bacteria without the use of drugs like antibiotics.
The bandage could help improve the quality of life of people who live with chronic non-healing wounds, which currently frequently require painful cleaning and treatment. Non-healing wounds can be a side effect of certain medications or health factors like diabetes, cancer or damaged blood vessels.
UV light is already widely used to sterilise objects like surgical equipment and fresh food. Treating bacterial infections in non-healing wounds with UV light instead of drugs could help to slow the rise of dangerous new strains of antibiotic-resistant bacteria known as ‘superbugs’.
In a new paper published in the journal IEEE Transactions on Biomedical Circuits and Systems, the researchers outline how they built the smart bandage and demonstrated its antibacterial effectiveness.
They built a slim, flexible inductive coil which could be integrated into the fabric of the bandage. The coil uses a technique called magnetic-resonant wireless power transfer to provide power to the UV LEDs without the need for batteries.
Instead, the inductive coil receives its power over the air, transmitted from a second coil connected to the electrical mains. The LEDs can be powered indefinitely simply by keeping the transmitting and receiving coils close to one another until the antimicrobial treatment is complete.
In lab tests, the researchers exposed samples of a strain of gram-negative bacteria called Pseudoalteromonassp. D41 to the UV light supplied by the smart bandage. Some forms of gram-negative bacteria can cause a range of serious infections in humans.
The tests showed that the smart bandage could slow and stop the growth of Pseudoalteromonas sp. D41 on the surfaces of slides, effectively eradicating the bacteria within six hours. The researchers suggest that the system could find use in medical settings to do the same for bacteria in patients’ chronic non-healing wounds.
“The use of ultraviolet light to kill viruses and bacteria is well known and this is the first work to integrate UVC emitting LEDs within a bandage and explore its efficacy. This approach could provide a significant benefit to the treatment of persistent wounds and is a major advance over typical smart bandages that attempt to monitor wound condition,” says Professor Steve Beeby, RAEng Chair in Emerging Technologies at the University of Southampton, who is a co-author of the paper.
Mahmoud Wagih, of the University of Glasgow’s James Watt School of Engineering, is another co-author of the paper. He developed the smart bandage’s wireless power delivery system.
“Traditional batteries are bulky, inflexible, and need to be changed regularly. That makes them difficult to use in bandages, which need to conform closely to the contours of patients’ bodies to deliver reliable treatment over several hours. The system we have developed is flexible and can be seamlessly integrated into the fabric of a bandage to power the LEDs, which deliver UV-C light across any surface,” says Wagih.
“We believe that smart bandages will be key to future healthcare, but we need to be mindful of their environmental footprint. In the UK alone, over 40,000 tonnes of batteries are sold annually and less than half of them are recycled. Our wireless power technology will allow healthcare wearables to grow, sustainably, as an alternative to drug-based treatments,” he adds.
“We will be continuing to collaborate on developing the bandage further to integrate sensors capable of monitoring the progress of wounds, as well as setting out to test the technology in clinical settings in the years to come,” he says.
The smart bandage is built on technology initially developed by Wagih and his colleagues from the University of Southampton. The research is showcased in a second paper, recently published in IEEE Transactions on Industrial Electronics.
The paper demonstrates the first use of magnetic-resonant wireless power transfer to provide electricity to standard textiles using embroidery or screen printing – a feature which helped to make the smart bandage possible.
In this case, the power was supplied to a newly-developed flexible electronic resistor made from silver and carbon which was printed into a textile surface to act as a wearable heating element. The system was capable of being heated to up to 60◦C while separated from the transmitter by 2cm at an efficiency exceeding 50%.
“Heaters are very power-intensive, so battery-powered heaters tend to either chew through batteries very quickly or provide only a moderate amount of heat for a bit longer before a change is required. This paper shows how high-frequency magnetic-resonant wireless power transfer can be used to power an efficient heating system built into clothing which can be washed and reused, which is impossible with conventional batteries,” says Wagih.
“The efficiency of power delivery is twice that of previous wearable wireless power receivers developed elsewhere. Given the importance of energy-efficient heating solutions, this opens up new possibilities for use in medical applications, heated clothing which could be worn in cold conditions, and more,” he explains.
Researchers from the Universities of Southampton and Glasgow in the UK contributed to the paper, along with colleagues from the Detection, Sensors and Measurements Laboratory at Infremer in France. The research was supported by funding from the Royal Academy of Engineering, the European Regional Development Fund Interreg France (Channel) England programme (Smart T project), the Engineering and Physical Sciences Research Council, and the Office of the Chief Science Adviser for National Security, says the statement.