Illegal mass sterilisation camps not a thing of the past
Experts say the pressures of family planning in India should not only be put on women (MIG photos/Aman Kanojiya)
In November 2014, Dr R K Gupta and an unnamed assistant carried out a record number of sterilisations of around 140 women in two camps in Chhattisgarh’s Bilaspur district. Gupta, known as a very senior and respected surgeon, had even been honoured by the Chhattisgarh government for achieving a record number sterilisations. A few days later, 15 women died, reportedly from blood poisoning and haemorrhagic shock. As many as 70 other women were hospitalised in critical condition, 20 of whom had to be put on mechanical ventilation. The law, then and now, only allows a maximum of 30 sterilisations per day.
The then-chief minister Raman Singh blamed negligence for the tragedy; medical committees were sent to investigate the incident and four health officials involved were suspended. Three separate fact-finding committees concluded that government norms were violated and the basic precautionary measures not taken. They found that the place where the operations were performed as well as the medical equipment used were not properly sterilised, and that post-operative care was almost nil.
However, Dr Gupta remained in jail for less than a month before he was out on bail, and in 2017, the Bilaspur High Court dropped all charges against him, despite challenges from patients and the deceased women’s families.
Dr Subhasri Balakrishnan works with Commonhealth and RUWSEC (rural women’s social education centre), non-governmental organisations working for women’s health and reproductive rights in India. She was part of the fact-finding committee made to investigate the 2014 sterilisation tragedy.
“There are a whole set of guidelines put in place by the Supreme Court for sterilisation camps, but these were not followed. And post the incident there really has not been any action against the persons responsible. First is the culpability of doctor, who had actually been awarded earlier for record number of sterilisations, but also the culpability of the system which encourages and incentivises doctors to perform such risky procedures,” Dr Balakrishnan tells Media India Group.
In the aftermath of the tragedy, the family planning programme in the state was totally shut down and women were denied permanent contraception. Seven years on, Chhattisgarh’s government medical officials seem to have learned nothing from the incident, with the health department carrying out tubectomy on 101 women in just 7 hours at a government mass sterilisation camp in Ambikapur on August 30; thankfully, there were no reported fatalities. Once again, a team of doctors has been formed to probe into the incident, but it remains to be seen whether justice will be served this time either.
Despite risks, women remain desperate
Like in 2014, the medical officers in charge at the Ambikapur camp once again claimed it was a helpless situation, due to the number of “adamant women” who refused to leave without the surgery.
But experts say that it is a fallacy to blame the women for engaging in such perilous medical procedures. According to the data from National Healthy Family Survey (NHFS-4), there is an inverse relationship between education and sterilisation in India. Due to a severe gap in information and lack of education, many women, especially in rural areas, go through the sterilisation procedure without fully understanding its significance and risks. Rather, they believe it is important to address why women in rural communities are so desperate for sterilisations in the first place.
“We have found in almost all parts of the country that women are desperate to have contraception in order to keep smaller families. However, because there is very poor access to any other contraceptive methods, such as regular supplies of pills, or IUCD services that are either not available or are of poor quality, women choose the only thing that is available, sterilisation,” says Dr Balakrishnan.
NHFS data since 2005 shows that the most popular form of contraception among both men and women in India is still female sterilisation, and perhaps most problematically, is significantly more prevalent than male sterilisation. In 2016’s National Policy for Women, the Ministry of Women and Child Development outlined a shift in focus from female to male sterilisation, but this policy has seemingly not been put into practice yet. According to latest NHFS-5 findings for example, in Andhra Pradesh where female sterilisation was the highest at 69.6 pc, male sterilisation was at a measly 0.4 pc. This is despite the fact that even when done correctly and in hygienic conditions, tubal ligation remains more risky and invasive than vasectomy.
“The matter of male sterilisation is nowhere in the picture because there are lots of misconceptions about it: how acceptable it is, worries about becoming weak, whether they will become impotent. It is also a larger issue within the patriarchal structure of Indian society; the responsibility of contraception falls on the woman, it is nowhere in the realm of male responsibility. Even though at the policy level, there is a push for vasectomy, on the ground there are just too many factors and barriers and I don’t think we are making a concerted effort to address them,” explains Dr Balakrishnan.
A dangerous bid for population control
Historically, India is the world’s first country to have a department devoted to family planning, with the government’s early emphasis on incentivised sterilisation in the 1970s, even encouraged by international organisations like the World Bank and the Ford Foundation.
But population control in the country is becoming an increasingly controversial issue, especially as some countries in Asia struggle with low birth rates. Uttar Pradesh’s 2-child policy, for example, was heavily debated by experts across the country. In 2016, the Supreme Court judgment, issued by a bench led by Justice Madan Lokur, called sterilisation camps “perverse products of the Centre’s population control campaigns driven by informal targets and incentives.”
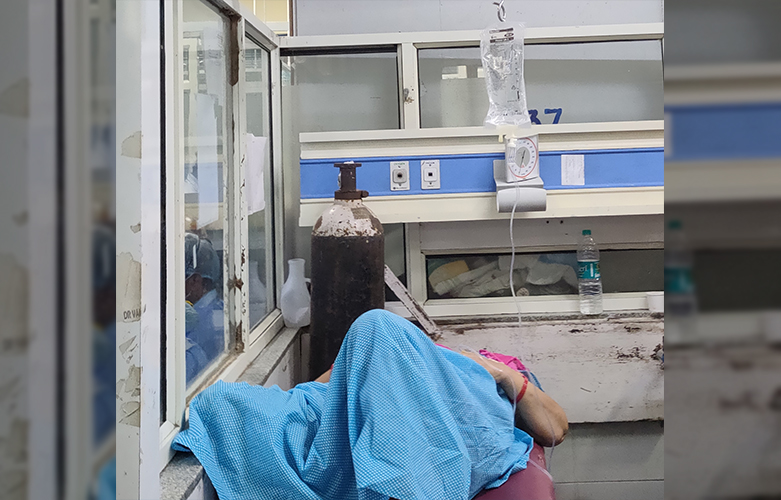
“If you look at states which have historically poorly-functional health systems, like Chhattisgarh, MP, UP, Jharkand, they do not have the capacity or resources to actually provide good quality care for any service. Many of the sterilisation camps have extremely poor quality of care; there aren’t enough beds so sometimes about 20 women lie waiting on mattresses in one ward. Often there are only 1-2 laparoscopic surgeons for the whole district, and they immediately leave after the operation, so post-operative care is left entirely up to the nurses or attenders, who may not be qualified to pick up on complications and address them,” says Dr Balakrishnan.
Healthcare experts say it is “horrendous situation” where women’s health is disregarded just to fulfill a government target.
“Most of the times, the procedure in these camps is done in a hurried, disorganised way, how else will you complete 100 surgeries in a day? But from a woman’s perspective, she is just taken in, brought out in this totally sedated state, and before she wakes up, everyone is gone. This is the general picture of how it happens, and it is very problematic. And a big reason something like this is going on is because of this population control discourse which talks about how the population is exploding and it needs to be controlled, and therefore anything to achieve that goal is acceptable,” she adds.
There are a number of other contraceptive methods that India’s healthcare system must wake up to in order to prevent more tragedies like 2014. Organisations such as ANM and ASHA, which are supposed to provide at-home contraceptive services such as condoms or oral contraceptives in rural areas, often are unable to do so as the supply chain is not maintained. The government and private medical facilities must take resolute steps to ensure that if population control or voluntary family planning is necessary, it must be done in a responsible and ethical manner.
“There are no concerted efforts to create good information sources that are accessible to women in a language they can understand, and which addresses their concerns. Women have no one to turn to if they face post-operative difficulties. Often sterilisation is seen as a one-time thing; get it done with and the headache is over, so that seems to be a deciding factor in women’s minds. There is definitely a demand for contraceptive services, but the health system does not seem to be fulfilling that demand with the provision of adequate supplies and services, so that is the thing that needs to be emerging, and this is true across the country,” says Dr Balakrishnan.









